Top 10 things to consider before reopening an ASC
Drew Garst, AIA, LEED AP
Elective surgery procedures are expected to resume in the near future. Certainly, changes need to be made to operations and facilities to accommodate this COVID-19 world. Below are some key recommendations to make ASCs safer and more efficient both in the near and long-term.
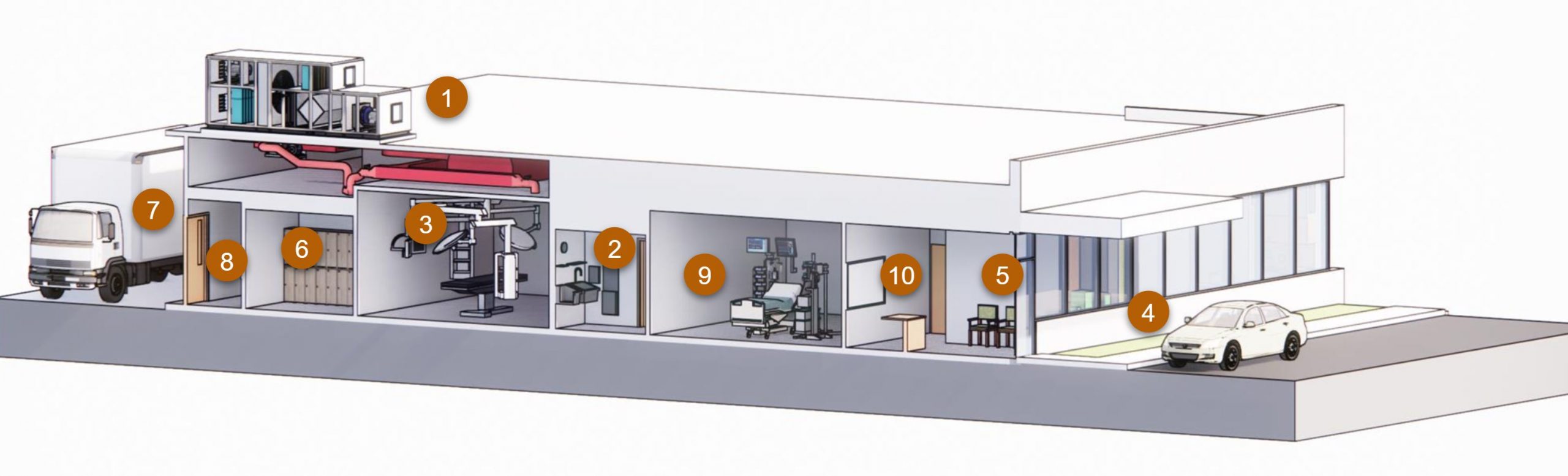
- When did you last replace your HVAC filters or check your duct work? Without the support of dedicated staff, facilities can sometimes struggle with basic maintenance. It is not uncommon for air filters to be kept in service well beyond their useful life. Facilities should validate that all pre and final filters are appropriate for continued use or have them replaced. There are guidelines from the National Institute of Health (NIH) and the American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE). This work can be done immediately while you wait for the 14-day all clear. COVID-19, and other airborne viruses, have been shown to harbor in HVAC systems and this is an opportunity to proactively address issues in your facility.
- How Good is Your Cleaning Service? Cleaning is often an outsourced service of an ASC. Now is the time to validate their work. Actively engage with the contracted company while they clean. This will ensure that they perform up to your specifications and do everything possible to reduce the infection risk in your facility. A routine audit of your cleaning company should be conducted on a regular basis moving forward.
- Are there repairs you have put off? Facilities commonly put off minor repairs. COVID-19 has provided some much-needed downtime to make these repairs that will benefit your facility well into the future. This is especially true in operating rooms. Many ORs suffer from worn out or damaged floors that are in need of repair. While seemingly minor, many of these issues put your patients at a greater risk of infection. Relying on the advice and experience of architects, interior designers, and contractors knowledgeable in healthcare facilities can help you determine if you only need to replace materials or if there are greater underlying issues that should also be addressed.
- Is using your Waiting Room really a good idea? One area that might see a new disproportionate stress in an ASC is the waiting room. Given the amount of resources it would take to make these rooms safe, facilities should strongly consider not using their waiting rooms at all. There are too many locations for the virus to take hold and too many people will be in close contact with one another. Instead, consider the following:
- Use Just-in-Time (JIT) software that integrates with your scheduling system to coordinate patient arrival. Several applications are on the market, such as Qminder that could significantly reduce the need for onsite waiting.
- Provide curb-side check-in and have patients wait in the vehicle until it is time to enter pre-op
- Encourage those helping patients before and after surgery to leave once the patient is taken into the facility.
- Use the same software to coordinate patient pick up after discharge.
- As much as possible, provide patient updates through digital platforms to keep friends and family members informed.
- What is the communication plan to your patients? Going into surgery under any circumstance is stressful for patients and family members. The COVID-19 situation has significantly heightened this stress and proactive steps need to be taken to help address that. A key strategy will be to document all the steps you have taken to ensure the health of everyone that uses your facility and then share that with the public. Communicate that you have sufficient PPE on hand, that supply chains are sustained and coordinated for safety, and the additional cleaning, preparation, and maintenance your facility has undertaken to ensure their safety.
- What safety measures are in place to protect staff? A protocol and dedicated space to evaluate staff health upon arrival is in order. In addition, it is not uncommon for staff to come and go to the facility in their scrubs. This is a hotly debated topic that covers both hygiene and professionalism. In the absence of empirical data as it relates specifically to COVID-19, it seems prudent to error on the side of caution. While it may be inconvenient, staff should come to work in street clothes, change into scrubs and leave in their street clothes when their shift is over. Developing a new staff arrival process to account for the enforced and modified procedures will help support staff and patient safety.
- Can you decrease touchpoints in your supply chain? We often don’t think about our supply chains until something breaks. COVID-19 has given us an opportunity to step back and ask some fundamental questions. An ASC needs to be vigilant regarding how things flow in and out of the facility. One great example is laundry. It is recommended that linens are handled as little as possible. Do you know how many handoffs your linens go through? This is both a question for internal staff as well as your vendor. While laundry service is just one supply chain component, it might be time to examine your entire system as we move into the post-COVID-19 ambulatory era.
- Can you implement small upgrades that decrease touchpoints? Small facility upgrades should also be considered at this time. One key factor to limit exposure is through hands–free technology. Adding auto operators to your doors will go a long way in reducing contact points. Most ASCs also outsource certain accessories such as paper towels, soap and hand sanitizer dispensers. Work with your suppliers to replace these items with hands-free options. Some of these items will need a little more ongoing support (such as battery replacement) and this is a good time to reset expectations with your suppliers about the type of support you expect.
- Can you flatten your own curve by decreasing density? This commonly used phrase may be useful as you determine the best way to reopen your ASC. While there is a backlog of elective surgery, the last thing any facility needs is an overstressing of their physical space, such as waiting rooms or pre– and post-op bays. ASCs should consider running on extended weekday hours and on weekends to limit the number of patients in the facility at any one time. This will limit most if not all waiting room stress and allow facilities the option to have patients use the same bay for pre– and post-op to limit turnaround cleaning needs. The implications to staffing needs will have to be addressed in conjunction with this concept, but these can certainly be overcome since it will enhance patient safety.
- What is your vision for the future? While the processes outlined here appear to be a response to the current COVID-19 situation, they may represent a new normal moving forward on how ASCs operate in the future. The awareness of the vulnerabilities of an at-risk population in a healthcare setting to infectious diseases may become part of a permanent re-shaping of our behaviors. Things such as minimizing touches, masking, the pervasive use of mobile technology, and even the possible demise of the waiting room as we know may become the norm. We can hardly remember a time when full-body scanners were not part of the airport experience, and that you once could meet your family at the gate. We now accept that the shoes, belt, jacket, water bottle-dance as an integral part of going through an airport. But with these inconveniences have come the innovations. Mobile ticketing, real-time updates to flight and gate changes, improved amenities at the gate level. This is our opportunity to plan for the future while we react to the present.