What Apollo 13 teaches us about quickly expanding our healthcare ecosystem for COVID-19
Drew Garst, AIA, LEED AP
In 1970, Apollo 13 astronauts Jim Lovell, John Swigert, and Fred Haise were thrust into a life and death situation after a routine cryogenic stir caused an explosion on their craft while on their way to the moon. With time as their enemy, the three astronauts worked with support from the ground to pull off the unimaginable. Through ingenuity and resourcefulness, they made it home while working only with the contents of the lunar lander Aquarius and the orbiter Odyssey.
During their ordeal, the astronauts did what they needed to do in order to survive, including rationing water to a meager 6 oz a day and suffering in a 38° F environment with little to keep them warm. They literally had to figure out a way to fit a square peg in round hole to remove life threatening CO2 from the lander. And in no small feat, mission control in Houston completely rewrote a new power–up sequence for the Odyssey in three days, something that typically can take up to three months. Every member of the team realized they had a finite amount of time to develop a plan, they knew that they needed to perfectly implement the plan, and they understood that there were severely limited resources to make it all happen.
For the United States to put our resources to best use during the coronavirus pandemic, we need to adopt the spirit, ingenuity, and innovation of the Apollo 13 team. What we have learned, particularly from countries like Taiwan and Singapore, is that quick response save lives. These governments acted quickly to manage their borders, had all necessary supplies ready to deploy, and put emergency response teams into action immediately. As the world watched the COVID -19 spread at a pace not seen in 100 years, this approach has proven successful in bringing the acceleration of cases down in a reasonable time.
In China, even though they were slow to react at first, they quickly pulled a plan together and set it in motion. China has a large share of the world’s construction supplies and the ability to put a robust workforce into motion overnight. That is why they were able to quickly prefabricate patient rooms and assemble two hospitals in two weeks. Now China is seeing their cases drop off and they have even closed the makeshift hospitals they just put into service. In contrast to this, is Italy. Their initial response was fragmented and inconsistent. To make matters worse, they lacked significant resources to scale up their healthcare system to manage or contain those infected. Most importantly, they were too late with moves like shutting down the rail system or lockdown, meaning that those measures shifted from the ability to contain the spread of the virus.
As a country, the United States cannot replicate the successes in Asia exactly as they did. The United States does not manage population health similarly on a national scale, relying instead on more local control, and to date, we lack the will to activate the required infrastructure to rapidly build new facilities on the scale we need in time. However, their success does give us a useful roadmap to follow. It suggests that our greatest chance of success needs to focus on three key elements: adopt the quarantine protocols, look for solutions based on assets we already have on hand, and implement a cohesive plan on a national level. As of April 1st, the reaction thus far in the United States has been too similar to that of Italy. Unfortunately, our rate of spread as indicated in Figure 1 is generating a steeper curve than in Italy, meaning that our peak is farther out and many more people will be infected by COVID-19. If we continue down this path, we need to understand that our outcome will be far worse than what we have seen in Italy. So, yes, Houston, we have a problem.
How do we respond?
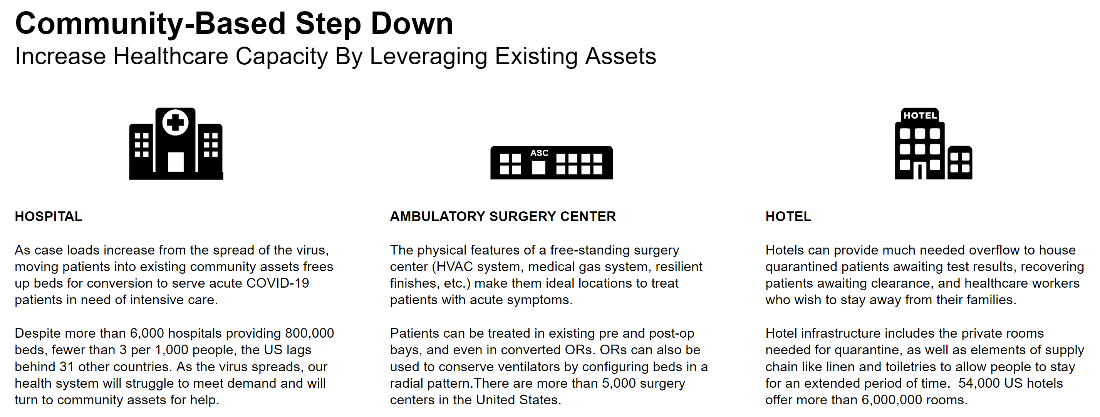
Like the Apollo 13 astronauts, time is the priority and we must work within the confines of our existing assets. On March 30th, the Centers for Medicare and Medicaid Services announced that they had waived a number of rules restricting care in facilities like ambulatory surgery centers, hotels, and dormitories that will now allow providers greater flexibility to treat patients. As we begin to develop a viable roadmap, here are some key elements to consider:
- According to the World Health Organization’s COVID-19 Situation Report 46, data to date suggest that 80% of infections are mild or asymptomatic, 15% are severe infection, requiring oxygen and 5% are critical infections, requiring ventilation. These fractions of severe and critical infection would be higher than what is observed for influenza infection.
- Hospitals, ASCs and hotels have a symbiotic relationship and often lie in close proximity to each other.
- The United States has a robust network of ASCs that are equipped and staffed with individuals capable of treating COVID-19 patients.
- Hotels offer private rooms with stand-alone HVAC systems. These could offer a certain level of support in managing the least vulnerable COVID-19 patients and limiting additional outbreak.
- Both ASCs and hotels are currently underutilized as portions of the United States have adopted shelter in place.
While the outline above does not capture the complexity of the situation, it does set the framework for how to solve the problem. Given where we are today, we offer the following as a starting point for a national response:
- Enact the more stringent quarantine policies that led to lower infection rates in Asia. Most of the United States has been informed of the benefits of social distancing, but our infection rate indicates the nation is not acting on this advice.
- Rapidly expand the physical footprint of our healthcare ecosystem to treat COVID-19 cases. In the immediate term, this should involve an expanded relationship between hospitals, licensed ASCs and hotels. Hospitals need to manage and operate with this expanded portfolio immediately. Local, state, and federal leadership need to enact this in unison.
- Hospitals and healthcare systems need to rework their triage criteria to understand how best to place patients in a larger system.
- Critical cases will stay within the traditional walls of a hospital. Assuming we can flatten the curve and critical cases stay at the 5% margin, our current healthcare system could theoretically absorb these patients.
- Mild cases will receive care in either an ASC or a hotel:
- ASC will take the severe cases where patients will be more vulnerable. ASC employ specially trained staff that have or may only require minimal training to treat COVID-19 cases.
- Hotels will house the least severe cases. Patients that are capable of self-preservation or might only require minimal remote monitoring could safely recover in this setting since there is a limited number of healthcare professionals available to provide any additional direct supervision.
- Leverage hotels to provide ancillary services.
- As the demand on hospital staff grows, healthcare workers will need to move around the country to provide support. Hotels can provide the necessary accommodations for mobile healthcare staff as the demand surge migrates throughout the United States.
- Containing the spread of the virus is still a critical component of our response. Hotels offer us the ability quarantine potential or susceptible portions of our population.
This is only the beginning of a universal plan to get us where we need to be, and we need to act with a sense of urgency to fill in the gaps. As a country we must be willing to adjust our environment which at times may be a little uncomfortable. We understand this outline only addresses the physical constraints of overcoming COVID-19. ASC and hotels are our Aquarius, they offer us the physical space we have available to expand our healthcare ecosystem.
Last week, the Defense Production Act was enacted to produce more ventilators. This will no doubt help the situation but, we need to find other solutions that are not time dependent. We believe there are like minded individuals that understand we need adapt a square scrubber into a round hole and have the expertise to so. And, this is not limited to ventilators. This applies to myriad other medical supplies that are needed on the front line, most notably Personal Protection Equipment (PPE). Hopefully we can find the missing pieces for our holistic response to this crisis. 50 years ago, America ingenuity brought Jim, John and Fred home. The United States needs to respond to the COVID-19 pandemic in that same spirit today.