How can ASCs be redeployed to increase healthcare capacity for COVID-19?
Drew Garst, AIA, LEED AP
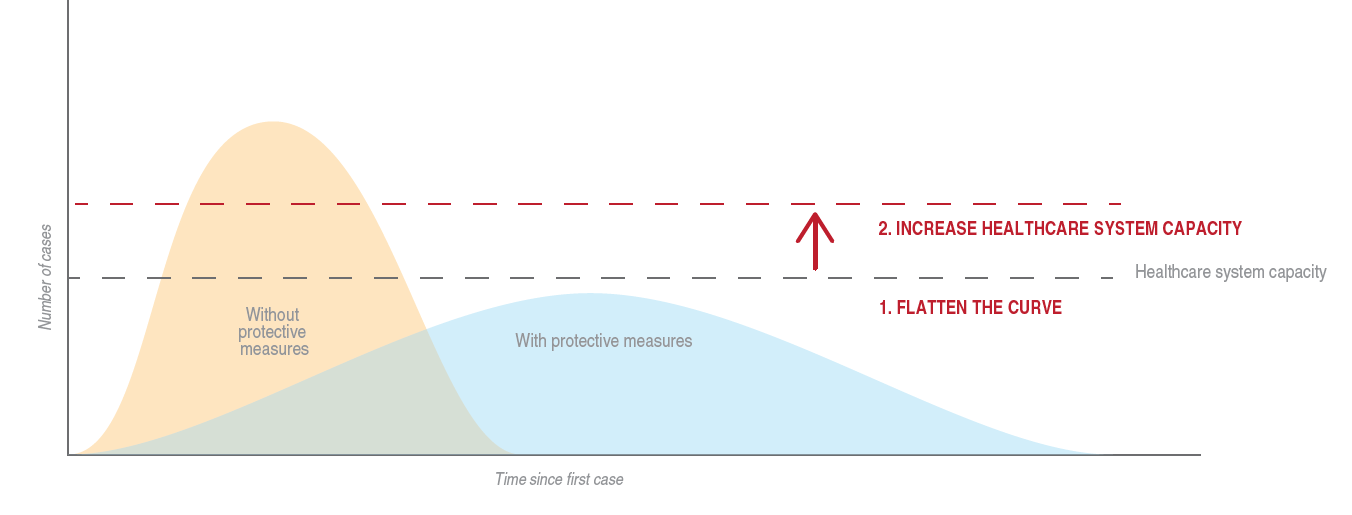
By now most of us are familiar with the “flatten the curve” diagram. The diagram also shows the curve relative to healthcare system capacity. In response to that, there is a lot of discussion right now about how the United States needs to increase hospital capacity to deal with the coronavirus. One of the ideas gaining traction is using prefabrication to construct new hospitals in a fraction of the traditional time. In heavily regulated states this could take three to ten years just to get 100 beds up and running. Most everyone watched in January and February as Wuhan, China took on the unprecedented task of putting together two prefabricated, ground up hospitals in two weeks. In total, they added 2,300 beds and the World Health Organization credits this accomplishment with saving lives. While the US discusses the logistical and regulatory requirements of replicating this achievement, we lose precious time. And, as many have already pointed out, there is the issue to get our prefabrication up to speed just to start putting hospitals together. Optimistic estimates put this at 90 days. So, while our country grapples with how to get this off the ground, we need to find make–ready solutions in the meantime.
ANALYSIS
Right now, the US has a unique asset in Ambulatory Surgery Centers (ASCs). These are typically independent facilities that perform outpatient surgery, commonly referred to as same-day surgery. According to the Ambulatory Surgery Center Association, we currently have 5,800 CMS-certified centers across the country. While these facilities are not equipped with all the bells and whistles of a hospital, they do carry all the necessary elements to help combat the coronavirus: HVAC systems with filtration, medical gases, handwashing stations, nurse stations, medication rooms and dispensing systems, emergency power and generators, the ability to safely run ventilators, cleaning and sanitation infrastructure, and life/safety features that make them safe for patient treatment. And even though many ASCs are not outfitted with overnight rooms, they do offer several spaces that can be put to immediate use.
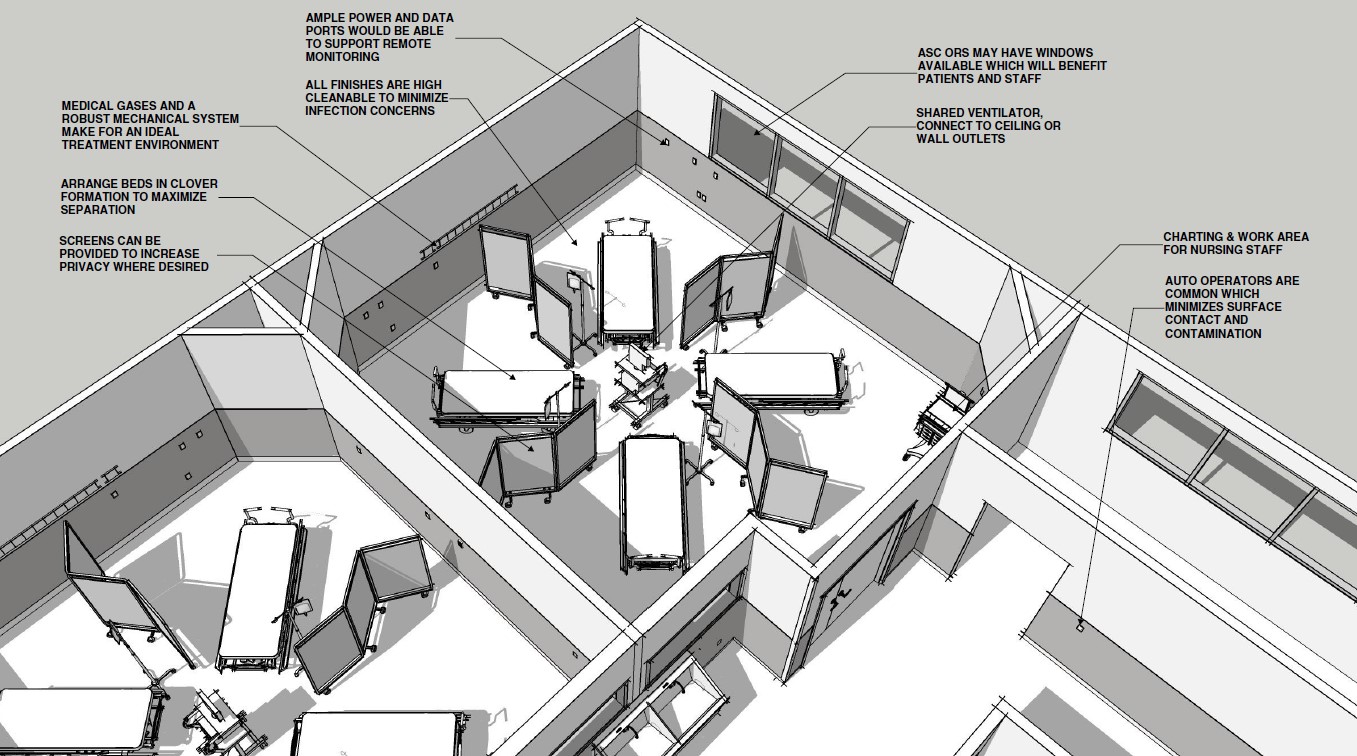
First, each facility is required to have Post Anesthesia Care Units (PACU). Every PACU must have the medical gases and emergency power that would be needed to treat COVID-19 patients. ASCs also have Pre-Op bays to prep patients before surgery. These spaces are not required by code to have gases but, often do to provide the surgery center with flexibility to manage the treatment of patients. The second potential space that could be used to treat patients is in the operating rooms (OR) themselves.
Though it is unlikely that all ASCs would suspend operations, it is possible to estimate the total potential capacity that could be generated. In the absence of hard data, we can use some rules of thumb to estimate the number of Pre-Op, PACU bays, and ORs in our country. First, we should look at the number of bays. Assuming the average center has three ORs with a minimum of three bays per OR, that is 52,200 additional spaces that could be put to immediate use. Since providers are increasingly cancelling elective surgeries, a further step would convert ORs into service for patient treatment. One compelling factor in this concept is the opportunity to conserve a critically limited resource, ventilators.
We have learned from one of our frontline partners that a shortage of ventilators will become a significant bottle neck in the treatment of COVID-19 patients. Luckily, they have developed a safe way to split a single ventilator to support as many as four patients. Since ORs are usually at least 400 square feet in area, this would give ample space to treat up to four patients at a time. To keep patient safety and facility flexibility for patient care in mind, we recommend leaving one OR open. So, at two ORs with four patients each, we can increase our capacity by an additional 46,400. This puts a total estimate of 98,600 new places to treat critically ill COVID-19 patients. If 2,300 new beds are credited with saving lives in China, imagine what the United States could do if we put 98,600 new spaces into services practically overnight. This additional capacity could help turn the tide in the fight of this epidemic.
RECOMMENDATIONS
The key to swift mobilization for this is to get several groups all moving in the same direction:
- ASC owners and operators need to be willing to open their doors and get their staff trained up to handle COVID-19 patients. In brief discussion with some of our ASC clients, they are ready and willing to step in during this crisis.
- Healthcare architects, engineers and contractors need to be ready to work with state and local jurisdictions to make any minor modifications to ensure patient safety is not compromised. In addition, state and local jurisdictions need to act quickly to allow this to happen. Code requires that ASCs have transfer agreements to local hospitals as part of their licensure. While this is not currently reciprocal, it could be quickly addressed by executive orders by governors.
- Hospitals and healthcare systems need to start working this new asset into their triage process. Knowing that this option is available will be key in pairing patients with the right level of treatment.
ASCs alone will not be able to stop the coronavirus but, they could be the strategic advantage the United States needs get a leg up on fighting this pandemic. They could be the stopgap while we work through all the issues of bringing additional beds online in the next six months.
This is an unprecendented event in Boulder Associates’ 37 years of providing design services exclusively for healthcare. We are here to offer to our particular knowledge and expertise in ASCs to providers as we battle this pandemic. Feel free to reach out to me at dgarst@boulderassociates.com.